Overview
Heart failure (HF) is currently classified using ejection fraction, but this measurement is limited and doesn’t reflect the many comorbidities often associated with managing patients with this complex condition.
Seeing an opportunity to better characterize patients with HF and encourage better approaches to clinical management, a team from Imperial College London used a model-based approach to cluster this U.S. population by comorbidities. They then compared clinical outcomes and health care utilization between the identified subgroups.
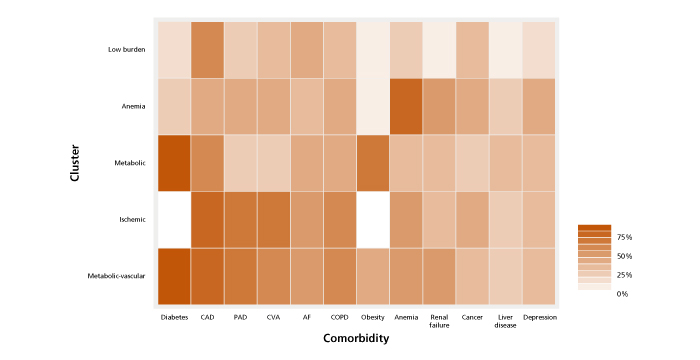
Five clusters with differential rates of hospital admission and mortality were identified: low-burden, metabolic-vascular, anemic, ischemic and metabolic.
The metabolic-vascular group had the worst prognosis; patients in this cluster were, on average, at double risk of hospital admission and had an 87% increased chance of death compared to the low-burden cluster, which served as the reference group.
This is believed to be the largest population-wide study involving data-driven model-based clustering in heart failure. The study was recently published in BMC Medicine.
Research
The Imperial team used administrative claims data in the OptumLabs® Data Warehouse from patients with commercial insurance or Medicare Advantage plans between 2008 and 2018.
They identified all individuals at least 18 years old with incident HF, defined as having at least one episode of acute HF that resulted in hospital admission, or at least two outpatient claims within the study period.
Latent class analysis was conducted using 12 comorbidities:
- Other cardiovascular conditions (atrial fibrillation [AF], coronary artery disease [CAD], peripheral artery disease [PAD], cerebrovascular accident [CVA])
- Metabolic conditions (diabetes mellitus, obesity)
- Depression
- Cancer
- Liver disease
- Renal failure
- Anemia
- Chronic obstructive pulmonary disease [COPD]
All models were adjusted for baseline characteristics: age, sex, race, education, medical insurance status, place of diagnosis (in- or outpatient), HF medications, and comorbidities not used in the clustering step: hypertension, alcohol misuse disorder, dementia and peptic ulcer.
Of the 318,384 patients with HF, the research team identified five comorbidity clusters, named according to their dominant features and characterized by different combinations of comorbidities and socio-demographic factors:
- Low burden: 93.4% had less than five comorbidities, with CAD being the most common (52.6% of patients).
- Metabolic-vascular: 99.7% had diabetes and 34.6% were obese. This cluster also had the highest percentage of HF prescriptions overall.
- Anemic: In addition to nearly all (96.4%) members having anemia, this cluster also had the highest proportion of women (63.7%), cancer (33.1%) and depression (26.4%).
- Ischemic: This was the oldest cluster (median age of 78), with a high prevalence of CAD (88.2%) and PAD (76.9%).
- Metabolic: This was the youngest cluster, with a median age of 67. All were diabetic and more than half (58.2%) were obese.
Clinical outcomes and resource use
All-cause hospitalization was the primary outcome of the study, defined as the first non-elective hospital admission with at least one overnight stay.
There was a direct relationship between number of comorbidities and increased risk for admission to the hospital. Those with over nine comorbidities were at triple the risk of being admitted to the hospital, compared to those with two or fewer comorbidities.
Overall, the metabolic-vascular group had the worst prognosis, with the highest risk of both hospital admission and death compared to the low-burden group. Conversely, the metabolic cluster had the lowest risk of admission or death. This group was the youngest, which may, in part, explain the more favorable prognosis.
The metabolic-vascular and ischemic clusters — the groups with the highest total number of comorbidities — were associated with similarly high risk for HF-specific hospital admission. These clusters also had the highest rates of cumulative length of stay, long-term care stays and office visits.
Cost differences mirrored health care utilization, with the metabolic-vascular cluster having the highest health care costs, followed by the ischemic cluster. Cost of care was primarily driven by inpatient and emergency room visits.
Opportunities for targeted intervention
These results suggest that the specific knowledge of how comorbidities cluster together and their association with clinical prognosis may assist clinicians who manage these complex patients to further refine and target their treatments.
The findings signal an opportunity for future clinical trials to enroll patients and test therapies based on prognostic comorbidity patterns, not just limiting them to ejection fraction treatment.
There is also a need for tailored comorbidity-management and prevention plans to accompany existing evidence-based medical therapy for patients with HF, in particular, targeting the clusters with the poorest prognosis.

